NHS compie 75 anni: Riflessioni sul BMJ
Il British Medical Journal celebra i 75 anni dell’NHS inglese con una domanda che ci interessa da vicino: cosa ci ha insegnato la pandemia rispetto ai benefici delle autonomie locali, e cosa andrebbe invece centralizzato?
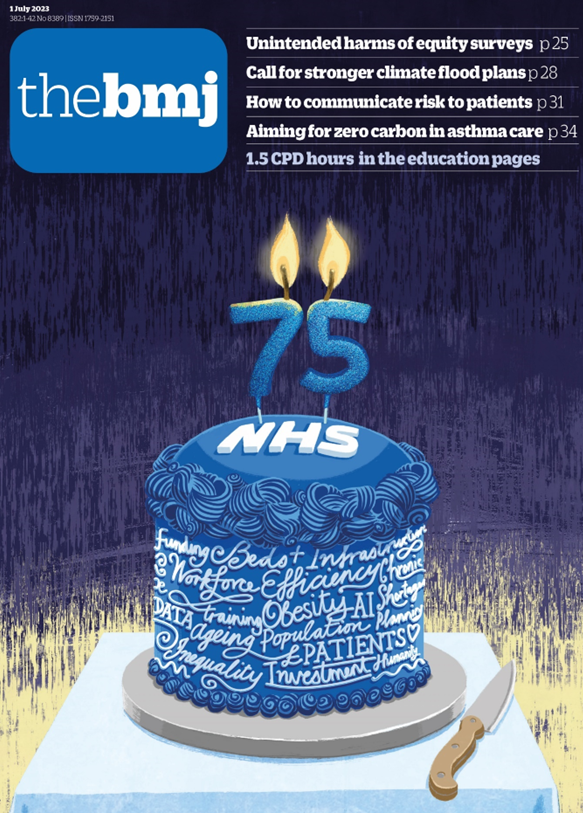
Il modello di base sul quale è stato costruito il Sistema Sanitario Nazionale italiano, ovvero l’NHS del Regno Unito, compie 75 anni. Nell’occasione, il British Medical Journal, rivista di riferimento assoluto per la sanità pubblica inglese e mondiale, dedica ampio spazio ad una serie di riflessioni, assai poco celebrative e con notevoli spunti critici.
I contributi editoriali si chiedono se in fondo si tratta di un buon compleanno1, e se il modello originale non andrebbe invece radicalmente trasformato per stare al passo con i tempi2. La problematica risulta ancora più complessa se si analizza quanto accaduto successivamente all’emergenza COVID-19, con i problemi ampiamente previsti di liste di attesa e personale sotto stress a causa degli alti carichi di lavoro, cui si aggiunge l’insoddisfazione dovuta ai livelli retributivi non commisurati all’effettivo costo della vita.
Eppure, nel NHS come anche in Italia, il modello a copertura universale sta resistendo, consentendo ai cittadini di restare al riparo dalle spese catastrofiche, che invece colpiscono le persone bisognose in altri Paesi altamente industrializzati, come nel caso più eclatante degli Stati Uniti.
I colleghi di Birmingham, R.Mannion e M.Exworthy, insieme agli esperti internazionali S.Wiig (Norvegia) e J.Braithwaite (Australia), si sono posti il problema di quale equilibrio possa essere raggiunto tra centralizzazione e decentralizzazione, in modo da affrontare nel migliore la fase di recupero dal COVID-193.
Ebbene, secondo gli autori la domanda va posta ricercando il giusto equilibrio tra livello di autonomia locale e centrale, imparando da quanto accaduto durante l’emergenza pandemica.
La tesi di Mannion e colleghi è abbastanza chiara: nel passaggio dalla emergenza alla ricostruzione, ovvero nella transizione da una fase in cui sono state delegate alcune funzioni importanti a livello locale per prestare servizi immediati alla popolazione colpita, ad un’altra di ripartenza pianificata, il rischio è quello di accentrare eccessivamente la politica sanitaria su base nazionale, rischiando di perdere tutti gli spinoff positivi generati dalla situazione di emergenza.
Durante l’emergenza COVID-19, sia nel Regno Unito che in Italia c’è stato un forte accentramento decisionale in aree fondamentali quali le politiche di lockdown, la distribuzione dei vaccini, il reperimento dei dispositivi di protezione individuale.
Al tempo stesso, a livello locale sono stati dispiegati processi molto efficaci per la popolazione, dando la possibilità agli enti locali di agire e sperimentare come mai accaduto prima (si pensi solo al teleconsulto e alla riorganizzazione rapida del personale).
Tutto ciò, secondo gli autori, ha una logica cristallina, in quanto la maggiore autonomia consente di agire più rapidamente, favorendo l’innovazione gestionale. D’altro canto, la centralizzazione delle politiche di finanziamento e la fissazione degli standard di performance possono rappresentare aspetti cruciali per garantire l’efficienza del sistema.
Secondo Mannion e colleghi, la “resilienza” (capacità di adattarsi alle mutate condizioni) necessita di garantire lo sviluppo dei servizi territoriali e sociali attraverso un convinto approccio solidamente ancorato alla partenza “dal basso”.
Certamente, rispetto al SSN italiano, l’NHS inglese è stato sempre storicamente più centralizzato, sia pure mostrando tendenze all’autonomia come nel campo delle “trust” ospedaliere e delle cure primarie.
La pandemia ha però impresso una accelerazione alle politiche di auto-determinazione, contribuendo ad aumentare la sensibilità verso responsabilità e decisioni locali, che hanno quindi favorito l’innovazione.
Per la crescita di entrambi i sistemi sanitari nazionali, è importante che questo patrimonio di esperienze e partecipazione responsabile non vada disperso.
Il monito che viene dall’articolo in questione è diretto alla capacità dei decisori centrali di capire che la volontà di essere autonomi deriva fondamentalmente dalla partecipazione attiva degli operatori della sanità ai processi di riforma.
Come dimostrano alcuni studi sul campo citati da Mannion e colleghi, il personale deve poter agire con tutta la flessibilità necessaria, per sfruttare appieno le proprie capacità organizzative capaci di dare risposte efficaci alle nuove sfide. In particolare, la “performance clinica di tutti i giorni” ha mostrato di funzionare con successo come rimedio a condizioni operative spesso inadeguate e confondenti per il personale coinvolto.
D’altro canto, la delega dei servizi a livello locale potrebbe non avere molto senso, se le risorse concesse risultano insufficienti e/o legate ad obiettivi di performance spesso irrealistici ed inconsistenti con gli obiettivi generali, generando delle incongruenze che di fatto finiscono con limitare la partecipazione attiva degli operatori.
L’implicazione principale è che le riforme non possono essere imposte dall’alto, affermando “cosa è necessario fare”, ma devono invece partire dal basso, chiedendo a ogni lavoratore “dove stai tentando di andare, e come possiamo aiutarti ad arrivarci”.
Secondo Mannion e colleghi, un aspetto cruciale per la promozione delle autonomie, è garantire il coinvolgimento di pazienti, pubblico e caregiver nel co-design dei servizi, realizzando quel sistema centrato sulla persona, di cui tutti parlano, ma che molti meno sono in grado di descrivere in termini di effettive condizioni operative.
Si tratta di aspetti studiati a fondo anche in Italia, ad esempio nel campo della valutazione partecipata, dove AGENAS ha messo a punto degli strumenti messi a disposizione delle Regioni e Province Autonome, che possono aiutare a standardizzare come misuriamo la centralità della persona nei servizi locali4.
Le riflessioni di Mannion e colleghi, a 75 dalla nascita del NHS inglese, ci offrono quindi una occasione per valutare criticamente quanto siano applicabili gli stessi principi per le nuove sfide di prossimità della cura in Italia.
Con i migliori auguri di buon compleanno all’NHS inglese.
- Riferimenti bibliografici:
- Walker I. The NHS at 75—a happy birthday? BMJ 2023; 381:p1460 doi:10.1136/bmj.p1460, https://www.bmj.com/content/381/bmj.p1460.
- Coombes R, Graham A, Leaf N, Pakunwanich N, Ugwuja J. Lifesaving yet frustrating, requiring transforming not dismantling—reflections on the NHS at 75 BMJ 2023; 381 :p1422 doi:10.1136/bmj.p1422, https://www.bmj.com/content/381/bmj.p1422.
- Mannion R, Exworthy M, Wiig S, Braithwaite J. The power of autonomy and resilience in healthcare delivery BMJ 2023; 382 :e073331 doi:10.1136/bmj-2022-073331, https://www.bmj.com/content/382/bmj-2022-073331.
- Cardinali F, Carzaniga S, Duranti G, Labella B, Lamanna A, Cerilli M, Caracci G, Carinci F. A nationwide participatory programme to measure person-centred hospital care in Italy: Results and implications for continuous improvement. Health Expect. 2021 Aug;24(4):1145-1157. doi: 10.1111/hex.13231. Epub 2021 May 20, https://onlinelibrary.wiley.com/doi/10.1111/hex.13231.